This article provides an in-depth guide to acid reflux, what it really is, the difference between GER and GERD, causes, symptoms, treatments, and parents’ frequently asked questions.

Acid, or gastro-esophageal, reflux is a common pediatric medical condition. Infants may exhibit crying with “spit-ups” after feedings, but the symptoms in toddlers and older children can be less obvious. Although some forms of acid reflux in babies and toddlers are normal, in many instances, it is a sign of a problem.
All About Acid Reflux in Babies and Toddlers
In this article:
- What is Acid Reflux?
- GER vs GERD In Infants
- What Are the Causes of GERD In Children?
- What Are The Typical Symptoms of GERD in Babies and Children?
- How is GER and GERD Diagnosed?
- How Is Reflux Treated?
- Prognosis: What Should Parents Expect?
- What If It Isn’t GER or GERD?
- How to Soothe Infants With GERD
- When to Call a Doctor
- Frequently Asked Questions About Acid Reflux in Babies and Toddlers
What is Acid Reflux?
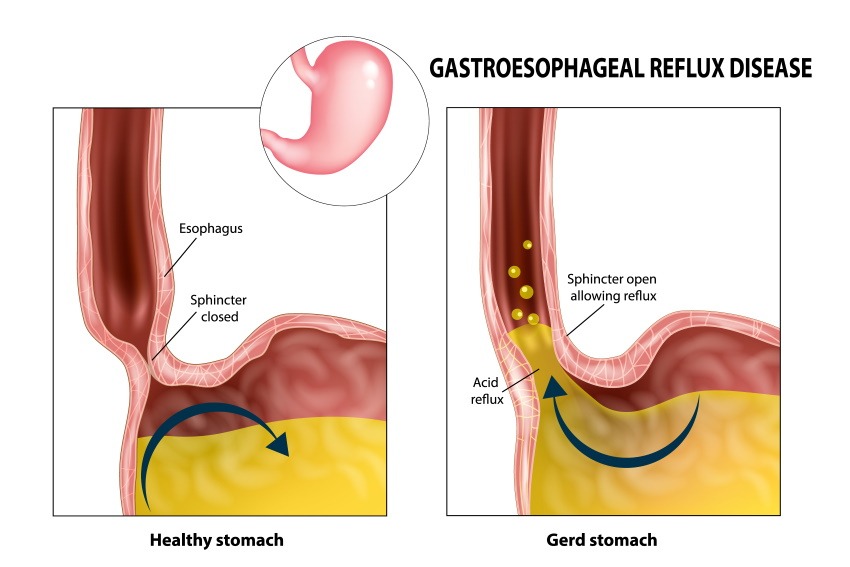
When an infant or child eats, the meal travels from the mouth, down the esophagus, and into the stomach. The muscle at the top of the stomach is called the lower esophageal sphincter. When fully functioning, it keeps food, gastric acid, and digestive enzymes within the stomach. If this muscle relaxes at other times, there can be a backflow of the stomach contents. “Acid reflux” is a general term used to describe this backflow when it is associated with discomfort.
In the pediatric population, reflux is divided into two categories: gastro-esophageal reflux (GER) and gastro-esophageal reflux disease (GERD). The former is very common in infants, and is considered normal. GERD, however, causes distress, and can be associated with other medical conditions.
The symptoms of GERD are different in each age group.
GER vs GERD In Infants
Lower Esophageal Muscle Immaturity
Many parents have had the experience feeding their baby, followed by some of breastmilk or formula returning out of the nose or mouth. The baby gently spits out some of the ingested milk with a burp, or when placed supine in a crib. The regurgitated milk may look slightly curdled, and it may seem as if the whole feeding has been lost. Despite this, the baby is happy, playful, and sleeps comfortably. This scenario is a typical case of normal infant GER.
Approximately 50 percent two month olds, and 70 percent of four month olds have GER episodes. The reflux occurs due to immaturity the lower esophageal sphincter. As the baby grows, the function of this muscle gradually improves throughout the first year of life. GER may completely resolve by age seven months for some infants, while others continue to have spit ups until their first birthday.
Despite its appearance, the amount of milk lost is negligible, and the expected growth parameters are achieved. This type of reflux is self-limited, and treatment is usually unnecessary.
Premature Birth
The organs of premature infants are underdeveloped, including the lower esophageal sphincter. As a result, the majority of premature infants experience GER or GERD. Diagnostic studies show that the lower esophageal sphincter relaxes many times throughout a 24 hour period, allowing reflux to occur. Nasogastric tube feedings can further impair this sphincter’s function, and exacerbate symptoms.
GERD is particularly stressful for premature infants. The sensation of the refluxed fluid itself, or the pain of acid irritation can trigger a drop in heart rate or pauses in breathing. Aspiration of the stomach contents into the airway can irritate the developing lungs, and cause permanent scarring.
Cow’s Milk Protein Allergy
Approximately three percent of infants are allergic to the proteins in cow’s milk. Infants are exposed via breastmilk if a mother consumes dairy, or from a cow’s milk-based formula. When ingested, these proteins can trigger an immediate reaction characterized by hives, facial swelling, vomiting, and wheezing. In most cases, however, symptoms are more insidious such as fussiness, frequent crying due to pain, and poor feeding. By the second to fourth week of life, streaks of blood usually appear in the baby’s stools due to intestinal irritation.
Studies show that approximately 40 percent of these infants also have GERD. Continued exposure to cow’s milk protein causes weight loss and poor growth.
Medical Conditions
GER or GERD can be associated with certain medical conditions. Some examples include Down syndrome, congenital organ malformations, and some neurological disorders. Sandifer syndrome is characterized by severe GERD symptoms along with abnormal body posturing and seizure-like movements.
In these complex cases, a multidisciplinary team is helpful in managing the both reflux and other aspects of the syndrome.
What Are the Causes of GERD In Children?
In the absence of an underlying medical condition, the lower esophageal sphincter should function properly in toddlers and older children. Although there may be periods of brief relaxation, food remains inside of the stomach most of the time. Therefore, the normal infant type of GER is rarely seen in this age group. When reflux does occur, it is symptomatic GERD, and there is a specific cause or contributing factor.
Constipation
Many children do not pass stools regularly or comfortably. This issue is particularly common in toddlers who are toilet training, but older children and adolescents may experience it as well. Low fiber diets and inadequate hydration are the primary triggers, but some children have inherent bowel motility problems such as Hirschsprung’s disease.
When the colon fills with stool due to infrequent evacuation, it causes gas accumulation. The gas distended colon exerts upward pressure against the stomach that is stronger than the lower esophageal sphincter. This causes reflux of the stomach contents, and, over time, irritates the esophagus.
Children may complain of “food coming up into the throat” or nausea when constipated. Managing the constipation and avoiding its triggers typically improves the associated GERD symptoms.
Diet
Certain foods are known to relax the lower esophageal sphincter, and exacerbate GERD. Caffeine in chocolate, teas, coffee, and soft drinks is a primary trigger. GERD is also more common in children who consume high fat diets or late night snacks.
Although many people believe that acidic and spicy foods cause GERD, in reality, they do not. These foods only make the child aware of the irritation caused by ongoing reflux.
Avoiding foods that relax the lower esophageal sphincter effectively reduces symptoms.
Obesity
Nearly 20 percent of children in the United States meet the criteria for a diagnosis of obesity. In addition type II diabetes, sleep apnea, and hyperlipidemia, GERD is common in children who are overweight. Both the upward abdominal pressure, and cytokines released by fatty tissue contribute to the development of GERD.
Weight loss measures can promote the resolution of symptoms.
Eosinophilic Esophagitis
This condition is characterized by chronic inflammation of the esophagus due to an abnormal immune response to foods or environmental allergens. Such exposures cause severe esophageal inflammation that can impair its contractions, and lead to permanent scarring. Eosinophils are the blood cells that proliferate during allergic reactions. They also release chemicals that relax the lower esophageal sphincter to produce GERD symptoms. This produces painful reflux and food regurgitation.
Treatment involves avoidance of the offending allergens, and managing the esophagitis symptoms.
Stress
Children often experience stress in their daily lives that produces physical symptoms. Midday headaches and stomach aches during school hours are common complaints. However, some children develop periodic nausea, vomiting, mid-chest pain, and night-time regurgitation. These symptoms may trigger sleep problems, anxiety, and/or depression . Heartburn pain itself can disrupt sleep, creating a cycle of daytime fatigue, stress, and stomach discomfort.
Stress management techniques and mental healthcare are both important in managing this type of GERD.
Pylori
Helicobacter pylori is a bacteria that can colonize the stomach. Pediatric cases most often occur due to transmission from adults in the household, or limited access to clean water. Although this illness is often asymptomatic, some children experience nausea, vomiting, and stomachaches. Left untreated, H. pylori increases the risk of stomach cancer.
In cases of persistent GERD, a test for this bacterial infection is often included in diagnostic workup.
What Are The Typical Symptoms of GERD in Babies and Children?
The symptoms of GERD differ for infants, children, and adolescents.
Signs in Full-Term Infants
- Feeds frequently, but takes several breaks during each feeding
- Frequent spit-ups with crying or irritability
- Crying in a supine position that resolves when held upright
- Frequent back arching
- Frequent sleep interruptions due to discomfort
Signs in Preterm Infants:
- Apnea -episodes where breathing stops
- Bradycardia -heart rate decreases to an abnormally low level
- Stomach distention
- Spit-up episodes
Note: some studies show that theses symptoms may not be triggered by reflux itself, but occur coincidentally.
Signs in Children:
- Nausea upon waking and prior to eating
- Decreased appetite
- Pain or a burning sensation in the mid-chest or upper abdomen
- Periodic vomiting in the absence of an infection
- Regurgitation and re-swallowing of stomach contents
- Frequent burping
- Weight loss
In severe cases, the pain worsens after eating, or there may be bloody vomiting. These are possible signs of a gastric ulcer, and warrant urgent medical attention.
How is GER and GERD Diagnosed?
Most cases of reflux are diagnosed based on clinical symptoms. Frequent “spit ups” are pathognomonic for infants with GER, but irritability, poor feeding, and sleep disruptions are signs of GERD. Coughing or wheezing may develop from micro-aspiration.
Toddlers and older children may complain of regurgitation, even when it is not visible to others. Morning nausea is common in grade school children which can result in a refusal to eat breakfast. Swallowing food can produce mid-chest discomfort. Complaints of “heartburn” pain are more common in older children, and can make lying flat in bed uncomfortable. Eating a meal may provide some temporary relief of mild GERD, but worsens the pain in severe cases.
On physical examination, pain may be elicited by pressing on the mid-epigastric area of the stomach, just below the rib cage. This is the location of the lower esophageal sphincter, and the pain reflects localized acid irritation.
Older children who experience frequent regurgitation may develop dental caries from acid erosion of tooth enamel.
Diagnostic tests are most often reserved for treatment refractory cases, or premature infants whose symptoms impair their hospital course. Tests are performed by either a pediatric gastroenterologist or neonatologist.
Multichannel intraesophageal impedance monitoring (MII)
MII monitoring is the diagnostic test of choice for preemies. An electrode catheter is inserted through the nasopharynx, and into the esophagus to measure the movement of fluids and air. It detects any back flow from the stomach into the esophagus.
Esophageal pH Probe Monitoring
This technique may be used in older infants and children to assess the severity of GERD. A catheter is inserted through the nose and lowered into the esophagus which detects the presence of stomach acid. Readings are taken over a 24 hour period, so a hospital stay is necessary.
Endoscopy
This procedure is the method of choice for diagnosing GERD caused by H. pylori . Under sedation, a tube with a camera is inserted from the mouth to the stomach, taking images and biopsies along the way. Non-invasive testing options include a PCR stool test of stool or a breath urea test. Blood tests are not particularly helpful, and only show the presence of H. pylori antibodies that developed at some point in the child’s life.
Endoscopy may be used in cases of treatment refractory GERD, and to diagnose eosinophilic esophagitis. The camera allows visualization of gastric ulcers, and severe esophageal inflammation. Biopsies may be taken to evaluate for pre-cancerous lesions.
Upper GI Fluoroscopy
In complicated cases, fluoroscopy may be used to identify medical conditions that mimic GERD. This is an x-ray guided imaging test during which a barium contrast liquid is swallowed. Real-time images are taken to capture any back flow of barium into the esophagus.
While it is helpful in ruling out other gastrointestinal abnormalities, this is not a first choice for infants and children with GERD.
How Is Reflux Treated?
The goal of treatment is to reduce symptoms that impair the quality of life, and to prevent longterm sequelae.
Management of GER
Most cases of normal infant GER do not require treatment. However, spit ups are messy, and a few strategies can make life easier for parents. These include:
- Avoiding a supine position for up to 30 minutes after a feeding
- Burping half-way through a feeding
- Giving smaller, more frequent feedings
These techniques allow ingested milk to flow via gravity along the baby’s gastrointestinal tract, and reduce the accumulation of swallowed air within the stomach. Babies may still have some episodes of GER, but they should be less voluminous and frequent.
If these measures fail, thickened feedings may be recommended by a doctor. Because of arsenic contamination of infant rice cereals, oat cereal is preferred for thickening expressed breastmilk or infant formula. As an alternative, there are infant formula options with added rice starch. This texture helps the feedings remain in the stomach, reducing the likelihood of reflux.
If using this method, it is important to discuss how to do it properly so that the feedings are safe. Adding too much cereal creates a choking hazard for babies.
Fortunately, normal infant GER self-resolves between the ages of six to 12 months. If it persists past the first birthday, this should be discussed with a doctor.
Management of GERD
Premature Infants
For many premature infants, GERD symptoms begin while they are receiving care in the neonatal intensive care unit.
Elevating the head of the hospital bed, and left side positioning can reduce reflux episodes.
In these situations, infants have cardiorespiratory monitoring, so episodes of apnea or reduced heart rate are easily detected.
Once a premature infant arrives at home, however, lying the baby flat on the back is the recommended safe sleeping position, regardless of GERD symptoms. Offering smaller, more frequent feedings can be helpful, but thickeners are not recommended due to the risk of necrotizing enterocolitis.
Although medications are sometimes prescribed for full-term infants and children with GERD, they have not been found to be safe or effective for premature infants.
Full-term Infants
Supportive care strategies are the first line of GERD treatment for full-term infants. As with normal GER, keeping the baby held upright for 30 minutes after feedings, frequent burping, and smaller feedings can reduce episodes. A trial of thickened feedings may also be helpful.
Under the mattress wedges and side sleep positions are not recommended, however, due to the risk of SIDS.
In some of these infants, GERD symptoms coexist with a cow’s milk protein allergy. Both improve when the cow’s milk exposure is eliminated. This may require a mother to withhold dairy from her diet while breastfeeding, or giving an extensively hydrolyzed (hypoallergenic) infant formula. A two to four weeks trial is typically recommended before moving on to other GERD treatments.
For GERD that is unresponsive to these measures, medication may be prescribed to reduce the pain of acid irritation. H2-receptor antagonists such as famotadine may be tried first, but are often less effective than proton pump inhibitor medications. These include omeprazole and lansoprazole which work by reducing amount of acid that is released by gastric cells into the stomach. Less acid present means less irritation of the esophagus. Although these medications reduce the discomfort of GERD, they do not stop the reflux itself.
Toddlers and Older Children
Lifestyle modifications are recommended for children who experience GERD symptoms.
If the BMI is elevated, weight loss can improve the muscle tone of the lower esophageal sphincter, and reduce reflux episodes.
Avoidance of foods that relax the lower esophageal sphincter can also help. These include caffeinated beverages or foods, and those containing peppermint. Spicy and oily foods move much slower through the gastrointestinal tract, and make reflux more likely.
Stress management and appropriate mental healthcare can improve GERD triggered by stress and mood disorders. A few studies have shown that chewing sugar-free gum after meals can reduce symptoms.
When lifestyle changes are ineffective, a trial of medication is warranted. Short-term relief may occur from antacid medications. They neutralize the stomach acid to prevent irritation. Antacids, however, should not be used longterm due to the risk of aluminum toxicity and adverse bone effects.
H2 receptor antagonist medications are the next choice for persistent GERD symptoms. These medications block the release of acid from some of the gastric cells, and can be helpful in mild cases. For example, a child who experiences morning nausea with decreased appetite for two weeks may have complete resolution of symptoms after a short course of an H2 receptor antagonist.
Proton pump inhibitor medications, however, are more much effective. Because of better gastric acid reduction, these medications promote healing of esophageal inflammation and gastric ulcers. They are typically prescribed for one to three months, depending on the severity of symptoms. If used longterm, the potential risk of bone fractures must be weighed against the benefits of reversing esophageal damage from GERD.
Special Situations
Children who are diagnosed with an H. pylori infection require treatment of both the infection and GERD. A three medication regimen has been established that includes an antibiotic, proton pump inhibitor, and a coating agent.
Amoxicillin has been the antibiotic of choice for many years, but resistance has developed. For this reason, a second antibiotic is often added to the regimen. Once H. pylori has been eradicated from the stomach, long-term complications are prevented.
In rare situations where GERD produces life-threatening symptoms, surgery may be recommended.
Certain neurological conditions, for example, are associated with lung aspiration from chronic persistent reflux. Infants with frequent apnea or bradycardia may benefit from a solution that stops the reflux.
If esophageal motility becomes impaired and constriction develops, a surgical solution is often necessary. A Nissen fundoplication is the most common procedure. Because gastric muscle can sustain very strong contractions, a portion of the upper stomach is used to encircle the lower esophageal sphincter and reinforce its ability to close. This prevents reflux of the stomach contents into the esophagus, thus eliminating GERD symptoms.
Unfortunately, a Nissen fundoplication is only functional for two to three years, and some patients ultimately require a revision.
Prognosis: What Should Parents Expect?
Most cases of normal infant GER self-resolve. 99 percent of infants outgrow it by their first birthday.
In the absence of an underlying medical condition, the majority of cases of GERD respond to lifestyle modifications or supportive measures. However, infants who experience GERD for more than three months are more likely to develop symptoms later during childhood.
What If It Isn’t GER or GERD?
At times, it may be difficult for parents to determine whether or not their infant is just spitting up or vomiting. The amount of milk expelled can often seem like quite a bit of a feeding has been lost. GERD and normal GER are typically characterized by casual dribbles or milk pouring out of the mouth. In contrast, vomiting is associated with a more forceful expulsion of the stomach contents. As vomiting continues, the fluid becomes a clear yellow or green color.
Most cases of vomiting are due to a gastrointestinal infection, however, there are a few conditions in which vomiting warrants immediate medical attention:
Pyloric Stenosis
This condition is characterized by very forceful, explosive vomiting. Parents often describe episodes in which the vomit “shoots across the room”. It is caused by an abnormal tightness of the muscle at the lower end of the stomach that prevents food from entering the small intestine.
It is more common in male infants, and the vomiting develops between ages three to five weeks of life. Failure to recognize this problem results in poor feeding, electrolyte imbalances, and weight loss.
Pyloric stenosis must be surgically corrected.
Bowel Obstruction
Any condition where the flow of food and fluids through the intestines is blocked can cause vomiting. Some infants are born with intestines that failed to fully develop in utero. In such cases, green (bilious) vomiting develops during the first few days of life.
An infant or child of any age can suddenly develop an intermittent twisting of the small intestines called a volvulus. In addition to vomiting, the twisting episodes are painful, and bloody stools are possible. Similar to this, infants or toddlers may develop a “telescoping” of an intestinal segment called intussusception.
Intermittent vomiting and abdominal pain can be intense, and mimic the symptoms of appendicitis. With the exception of intussusception, most bowel obstructions require surgical intervention.
Abdominal Migraines
Some toddlers and children experience chronic episodes of intense abdominal pain with nausea, vomiting, and poor appetite that self-resolve. Although some children have concurrent headaches, many do not. Symptoms develop between ages three to 10, and there is usually a family history of migraine headaches.
Parents and children are taught to recognize and avoid the triggers of abdominal migraines, and medication is rarely necessary.
How to Soothe Infants With GERD
The amount of discomfort some babies with GERD experience can be quite distressing for parents. Their infant cries throughout the day and night, has difficulty sleeping, and is often difficult to console. Witnessing these symptoms can become stressful for parents, exacerbating feeding difficulties, and impairing bonding.
In addition to supportive measures, pacifiers can be particularly helpful for soothing younger infants. For others, swaddling and “white noise” sounds can have a calming effect at nap and bedtimes. Swaddling, however, should be discontinued once a baby tries to roll over which is a SIDS risk.
The inclined position and motion of an infant swing may have a calming effect during awake hours.Doing “tummy time” often provides some temporary relief while practicing developmental skills.
If, despite these measures, the GERD symptoms persist, a discussion with a doctor about medications is warranted. Although research studies have not proven that H2 receptor antagonists and proton pump inhibitors block the pain, many infants appear to have less discomfort when they are prescribed.
When to Call a Doctor
Some symptoms are not simply GER or GERD, and medical attention is necessary. These include:
- Vomiting with fever
- Vomitus that is clear yellow or green
- Lethargy or the baby is difficult to arouse
- Vomiting with diarrhea
- Forceful vomiting
- Blood in stools
- Poor feeding for over 12 hours
- Poor weight gain despite regular feedings
For toddlers and older children, the following symptoms warrant emergency evaluation:
- Persistent vomiting and/or diarrhea
- Vomiting blood
- Vomitus that is clear yellow or green
- Abdominal pain that is severe or worsens over time
- Blood in stools
- Fever with abdominal pain (possible appendicitis)
Speaking with a doctor helps determine if the issue can be managed in an office setting, or when hospital care is needed.
Frequently Asked Questions About Acid Reflux in Babies and Toddlers
Is there a difference between GERD and acid reflux?
No. Acid reflux and GERD are essentially the same condition, associated with uncomfortable reflux of the stomach contents. Mid-chest or upper abdominal pain occurs along with regurgitation into the upper esophagus or mouth. In contrast, GER is the normal type of “spit up” that many babies experience.
What is silent reflux?
Silent or laryngopharyngeal reflux is characterized by a backflow of the stomach contents to the throat level, but with upper respiratory symptoms. Children may present with a chronic intermittent cough, hoarse voice, or throat clearing. The reflux typically occurs during the daytime or with burping, and rarely while lying flat. Unlike GERD, esophageal inflammation is rare, but throat irritation may be present. This condition is usually treated with proton pump inhibitor medications.
Are there foods I should avoid giving my baby/toddler with acid reflux?
Mothers who are breastfeeding should avoid caffeinated beverages. This ingredient is transmitted to babies via breastmilk and relaxes the lower esophageal sphincter. If a baby or toddler has been diagnosed with a cow’s milk protein or other food allergies, such foods should be avoided as well.
Toddlers who are able to communicate feelings of stomach or chest pain may have fewer symptoms if acidic or spicy foods are kept out of their diets. These foods can be uncomfortable to eat when the esophagus is irritated.
Does gripe water help with acid reflux? Why or why not?
No. Gripe water has not been shown to reduce the discomfort of GERD or colic in clinical studies. It may also cause vomiting or constipation in infants. In addition, the formulations of gripe water are inconsistent, and some products may have bacterial contamination.
Does warm milk help with acid reflux in babies? Why or why not?
Breastmilk or formula, at any temperature, can soothe the “burn” of acid irritation in the esophagus. There is no difference in the effect when offering it warm, at room temperature, or cold.
What feeding schedule changes should I make for my acid reflux baby?
Smaller, more frequent feedings may reduce the volume of “spit up.” For example, if a three-month-old infant consistently has GER after consuming a 4oz bottle every three hours, there may be less reflux when offered 3oz every two hours.
A smaller amount of milk in the stomach is less likely to reflux into the esophagus, even in the presence of swallowed air. This smaller volume of milk easily passes into the intestines and leaves less residual milk in the stomach.
Should I stop breastfeeding when my baby has acid reflux?
No. GER or GERD are not a reason to stop breastfeeding. However, if your infant has been diagnosed with a food allergy, your pediatrician may recommend withholding certain foods from your diet.
My toddler has acid reflux at night. What shall I do?
Five percent of toddlers continue to have reflux at 12 months old. Although a discussion with a doctor is warranted, lifestyle modifications may be recommended for another year. Symptoms after age two, however, are atypical and warrant further evaluation .
My baby throws up when pooping. Is this a sign of acid reflux?
Vomiting while stooling (normal or diarrhea) is unusual, and not associated with GERD. If your baby does this consistently, you should contact a doctor.
Takeaway
This is quite a long and thorough guide to acid reflux in babies, toddlers, and older children. In most cases, especially with babies, some acid reflux and spitting up is completely normal. Nevertheless, it is important to address signs of GERD or other issues if suspected.
Hopefully, this article has given you either comfort or some ideas on ways forwards to help your child.
If you have any questions or experiences to share, post them in the Comments below.
Good luck!
Read next
- Baby Spitting Up Curdled Milk: 10 Important Reasons to Check
- Help, Baby Gasps When Laid Down! 11 Reasons to Investigate
- Signs Of Milk Protein Allergy or Lactose Intolerance In Toddlers and Babies
- My Baby Is Crying All The Time: Colic, Reflux or What..?
Research References
- Gastroesophageal Reflux: Management Guidance for the Pediatrician
- Gastroesophageal reflux in children: an updated review
- Patient education: Acid reflux (gastroesophageal reflux) in infants (Beyond the Basics)
- Diagnosis and Management of Gastroesophageal Reflux in Preterm Infants
- Dietary habits and gastroesophageal reflux disease in preschool children
- Diagnosis and management of Sandifer syndrome in children with intractable neurological symptoms
- The role of diet in the development and management of gastroesophageal reflux disease: why we feel the burn
- Obesity and its effects on the esophageal mucosal barrier
- What are cytokines?
- The overlap of gastroesophageal reflux disease and functional constipation in children: the efficacy of constipation treatment
- Childhood Obesity Facts
- Gastroesophageal Reflux Disease and Eosinophilic Esophagitis
- Heartburn in children and adolescents in the presence of functional dyspepsia and/or irritable bowel syndrome correlates with the presence of sleep disturbances, anxiety, and depression
- Pediatric eosinophilic esophagitis: a review for the clinician
- Functional constipation in children: challenges and solutions
- What are Peptic Ulcers?
- Helicobacter pylori Infection in Children: a Comprehensive Review
- Oatmeal: The Safer Alternative for Infants & Children Who Need Thicker Food
- What Is Necrotizing Enterocolitis?
- Histamine H2 Antagonist (Oral Route, Injection Route, Intravenous Route)
- Prevalence and Parental Perceived Efficacy of Rice Cereal in Bottles Used as a Natural Sleep Aid for Infants Aged 0-11 Months
- What is Nissen Fundoplication?
- What is Pyloric Stenosis?
- What Is Intussusception?
- Congenital Neonatal Intestinal Obstruction
- What is Volvulus?
- Gripe Water Administration in Infants 1-6 months of Age-A Cross-sectional Study
- Laryngopharyngeal Reflux: A State-of-the-Art Algorithm Management for Primary Care Physicians
- Pediatric abdominal migraine: current perspectives on a lesser known entity

Paula Dennholt founded Easy Baby Life in 2006 and has been a passionate parenting and pregnancy writer since then. Her parenting approach and writing are based on studies in cognitive-behavioral models and therapy for children and her experience as a mother and stepmother. Life as a parent has convinced her of how crucial it is to put relationships before rules. She strongly believes in positive parenting and a science-based approach.
Paula cooperates with a team of pediatricians who assist in reviewing and writing articles.