One of the first questions many parents ask after a miscarriage is: “Why did this happen?” At the same time, many women in early pregnancy worry: “What if I do something that causes a miscarriage?”
Both questions are natural. Miscarriage is the most common type of pregnancy loss, and yet it is often misunderstood. The truth is that most miscarriages happen because of factors outside anyone’s control. In fact, doctors cannot identify a clear reason in many cases.
Understanding what actually causes miscarriage—and what does not—can help bring clarity, reassurance, and sometimes peace of mind.
My Story
When I first became pregnant, I (sort of) thought it would feel like the advertisements – carefree women glowing and enjoying every moment. The reality was very different. Every twinge, cramp, or spot of bleeding made me worry and wonder if I was miscarrying. I found myself counting the days until that magical first heartbeat, and then again until the end of the first trimester.
If you’ve felt the same way, you’re not alone. Miscarriage is something many of us fear, but as I learned, most pregnancies continue normally, and the things we often blame ourselves for are not usually the cause.
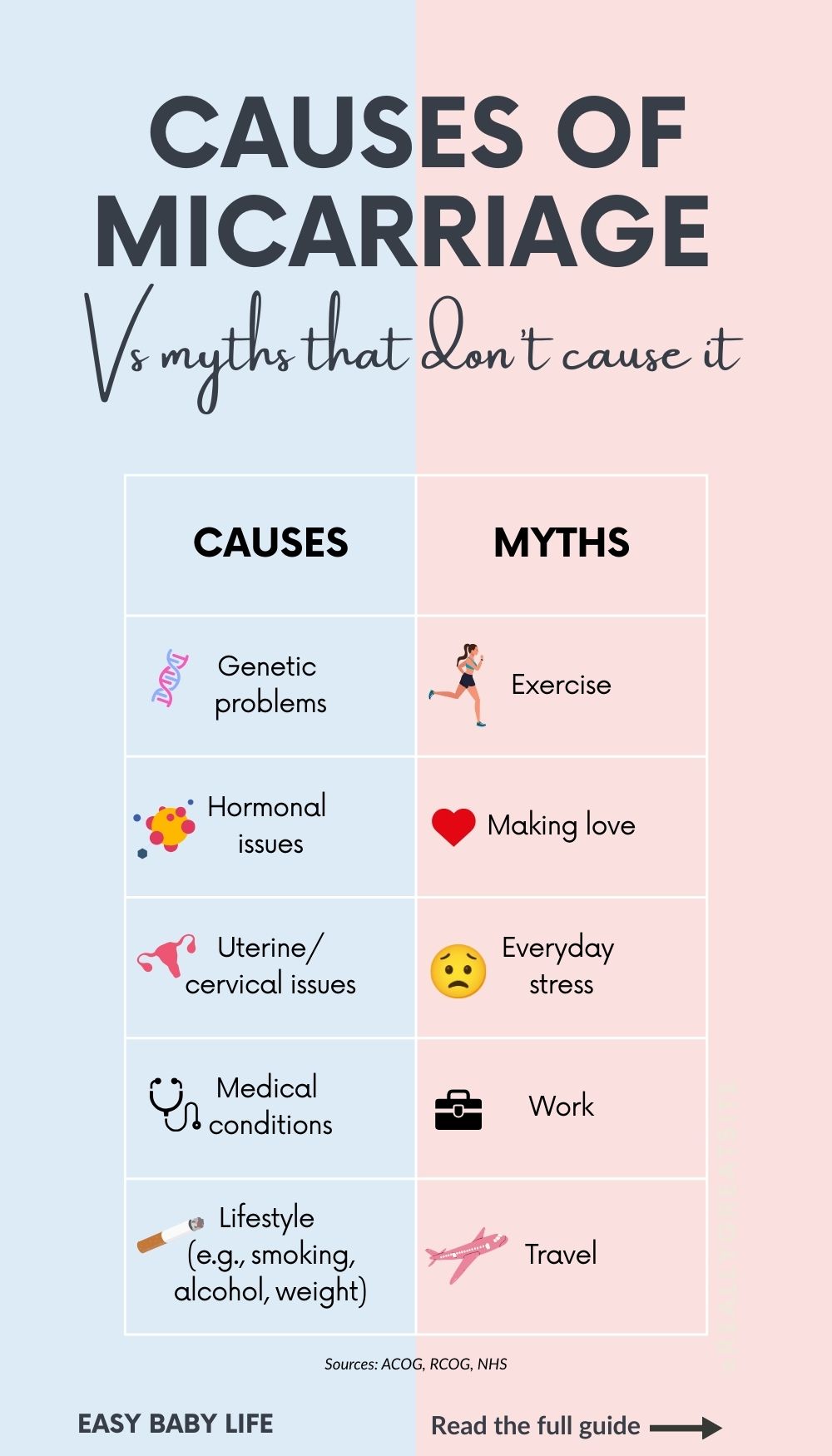
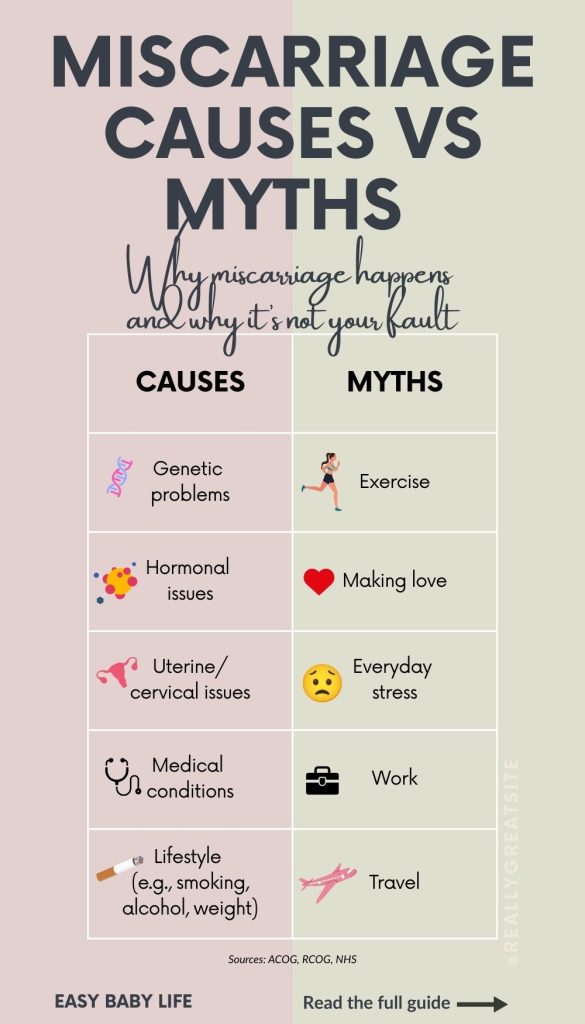
1. Genetic Causes (The Most Common Reason)
By far, the most frequent cause of early miscarriage is genetic problems in the embryo. Researchers estimate that around 50–60% of first-trimester miscarriages occur because of chromosomal abnormalities.
This usually happens by chance when the egg and sperm come together. Instead of the normal 46 chromosomes, the embryo may have too many or too few. Some common examples include:
- Trisomy: an extra chromosome, such as trisomy 16 (not compatible with life).
- Monosomy: a missing chromosome, such as Turner syndrome (a single X chromosome).
- Translocations: parts of chromosomes breaking and rearranging.
These abnormalities prevent the embryo from developing normally and lead the body to stop the pregnancy. Importantly, these are almost never caused by anything a parent did.
The risk rises with maternal age. For example, studies show the risk of miscarriage is around 10–12% at age 20–30, about 18% at age 35, and increases to over 50% by age 42.
2. Hormonal and Anatomical Causes
Some miscarriages are linked to hormone balance or the structure of the uterus.
For example, progesterone is often called “the pregnancy hormone.” It helps prepare and maintain the uterine lining so an embryo can implant and grow. If progesterone levels are too low, implantation or early development may fail. Similarly, untreated thyroid problems (an underactive or overactive thyroid) and polycystic ovary syndrome (PCOS) have both been linked with higher miscarriage risk.
Uterine and cervical issues can also contribute:
- A uterine septum (a band of tissue dividing the uterus), significant fibroids, or scarring from surgery may interfere with blood supply.
- A weak or short cervix (cervical insufficiency) can open too early, usually in the second trimester. This can lead to pregnancy loss (sometimes classified as a late miscarriage, depending on timing and country definitions) or very preterm birth.
In some cases, implantation problems in the uterine lining may prevent a pregnancy from developing.
These causes are less common than genetic issues, but many can be diagnosed and sometimes treated.
3. Lifestyle and Environmental Factors
It’s natural to wonder if lifestyle habits played a part, but for most people, these are not the main cause of miscarriage. Still, research shows that certain factors can increase risk:
- Smoking: linked with a higher rate of miscarriage and pregnancy complications.
- Alcohol: heavy use clearly increases risk; most guidelines advise avoiding alcohol entirely during pregnancy.
- Body weight: Being significantly overweight (BMI >30) or underweight (BMI <18.5) may affect hormones and increase miscarriage risk.
- Caffeine: Most guidelines recommend limiting to ≤200 mg/day. This equals about:
- 1 large 12 oz (350 ml) cup of brewed coffee (≈180 mg), or
- 2 medium 6 oz (180 ml) cups (≈95 mg each).
Remember that tea, soda, and chocolate also add caffeine.
- Environmental exposures: Radiation, certain industrial chemicals, and heavy air pollution may raise risk in rare cases.
Stress is often blamed, but here the research is mixed. Some studies suggest extreme, repeated traumatic stress may increase risk, but most evidence shows that everyday stress, anxiety, or worrying does not cause miscarriage.
4. Medical Conditions and Infections
Certain underlying health conditions can play a role in recurrent or later miscarriage.
- Diabetes: Poorly controlled blood sugar levels increase risk. With good management, risks are close to normal.
- Heart disease, thyroid disease, and autoimmune disorders can sometimes reduce uterine blood flow, limiting oxygen supply to the fetus.
- Autoimmune conditions, such as antiphospholipid syndrome (APS), can cause blood clotting that interferes with the placenta. Once diagnosed, APS is often treated with blood-thinning medication such as heparin or aspirin.
- Blood disorders: Some clotting disorders (inherited or acquired) can increase risk.
- Infections: Most common infections—like colds or mild flu—do not cause miscarriage. But certain untreated infections (such as listeria, toxoplasmosis, or rubella) may be linked. These are now rare in countries with vaccination and food safety measures.
5. Unknown Causes
Even with thorough testing, many miscarriages remain unexplained. This can be one of the hardest things to accept.
Doctors believe many of these are due to genetic problems we cannot yet detect. The important reassurance is that an unexplained miscarriage does not mean you are unhealthy or that you won’t have a successful pregnancy in the future. In fact, most women who have one or even two miscarriages go on to have healthy babies.
6. What Does Not Cause Miscarriage (Common Myths)
Many parents blame themselves after a miscarriage. But research shows that everyday activities almost never cause pregnancy loss.
- Exercise: Light to moderate physical activity, including walking, yoga, and most fitness routines, is safe.
- Sex: Intercourse does not cause miscarriage in a healthy pregnancy.
- Work: Most jobs, even active ones, are safe unless there is exposure to toxins or extremely heavy lifting.
- Travel: Flying and car trips are safe in early pregnancy.
- Everyday stress: Feeling anxious, worried, or tired does not cause miscarriage.
- Coffee: Staying under 200 mg/day is considered safe (≈ one large cup or two medium cups – see cup sizes above).
If you’ve had a miscarriage, it’s important to know: it wasn’t your fault.
7. When to Seek Medical Advice
If you are pregnant and worried about miscarriage
Contact your healthcare provider if you notice:
- Vaginal bleeding (especially heavy or with clots).
- Strong cramping or abdominal pain.
- A sudden loss of pregnancy symptoms (such as nausea or breast tenderness).
- Passing fluid or tissue from the vagina.
Your doctor or midwife may recommend an ultrasound or blood tests to check the progress of the pregnancy.
If you have recently had a miscarriage
Seek urgent medical attention if you experience:
- Very heavy bleeding (soaking through a pad in an hour),
- Severe abdominal pain,
- Fever, or
- Foul-smelling discharge.
These may be signs of complications, such as infection, that require medical care.
If you’ve had repeated miscarriages or have underlying health issues
One miscarriage is usually considered a chance event. But if you experience two or more in a row, or if you have medical conditions like thyroid disease, diabetes, or blood clotting disorders, it’s a good idea to see a doctor. They may recommend tests such as blood work, hormone checks, or imaging of the uterus to look for underlying causes.
Conclusion

Most miscarriages happen because of genetic problems in the embryo, and nothing could have been done to prevent them. In other cases, hormone balance, uterine health, or medical conditions may play a role—but many miscarriages remain unexplained.
What’s equally important to remember is what does not cause miscarriage: exercise, sex, work, travel, everyday stress, or a safe amount of coffee.
Miscarriage is not a punishment or a sign you did something wrong. In fact, many experts believe it is sometimes nature’s way of ensuring that only healthy pregnancies continue. This doesn’t make the loss any easier, but it may help relieve feelings of guilt.
If you have experienced a miscarriage, please know you are not to blame. And if you are pregnant and worried, remember that most pregnancies progress normally. The chances of having a healthy baby are very high.
Perhaps all of this scary and very real pregnancy information on what can cause a miscarriage begs the realization that pregnancy can be stressful, difficult emotionally, and overwhelming. THAT is also known as parenting – and it begins at conception.
Unfortunately, it doesn’t seem to become any easier either – there will always be more things to worry about and more things we wish we could control. So, try to sit back and enjoy the ride to motherhood.
Or, as a midwife told a friend of mine who complained about worrying so much: Get used to it! The worrying will not stop until your adult child moves out – or actually, it will not end ever.:-)
Related Reading
- Miscarriage Statistics By Week
- Getting Pregnant After Miscarriage
- Having A Period While Pregnant – Possible?
References
- Tong S, Kaur A, Walker SP, Bryant V, Onwude JL, Permezel M. Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit. Obstet Gynecol. 2008 Mar;111(3):710-4.
- Wilcox AJ, Weinberg CR, O’Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med. Jul 28 1988;319(4):189-94.
- Allison JL, Schust DJ., Recurrent first trimester pregnancy loss: revised definitions and novel causes. Curr Opin Endocrinol Diabetes Obes. 2009 Dec;16(6):446-50.American College of Obstetricians and Gynecologists (ACOG). Early Pregnancy Loss. Practice Bulletin No. 200, 2018.
- Royal College of Obstetricians and Gynaecologists (RCOG). Recurrent Miscarriage: Investigation and Treatment. 2011.
- Rai R, Regan L. Recurrent miscarriage. Lancet. 2006;368:601–611
- Nybo Andersen AM, et al. Maternal age and fetal loss: population-based register linkage study. BMJ. 2000;320:1708–1712.

Paula Dennholt founded Easy Baby Life in 2006 and has been a passionate parenting and pregnancy writer since then. Her parenting approach and writing are based on studies in cognitive-behavioral models and therapy for children and her experience as a mother and stepmother. Life as a parent has convinced her of how crucial it is to put relationships before rules. She strongly believes in positive parenting and a science-based approach.
Paula cooperates with a team of pediatricians who assist in reviewing and writing articles.